
The concern is that the Triple Aim is lacking a fourth fundamental element the Triple Aim fails to acknowledge health care workers’ critical role in delivering on the initial three aims. Nine years later, many providers within the health care industry believe it is time to modernize the concept. Since 2007, the IHI’s Triple Aim has symbolized health care’s patient-centered focus. IHI further believes that in order to do this work effectively, it is important to harness a range of community determinants of health, empower individuals and families, substantially broaden the role and impact of primary care and other community-based services, and ensure a seamless journey across the system of care throughout a person’s life.įinally, it is thought that the Triple Aim can be a foundational element of many areas of health reform, including accountable care organizations, bundled payments, and other innovative financing approaches new models of primary care, such as patient-centered medical homes sanctions for avoidable events, such as hospital readmissions or infections and the integration of information technology. The initiative calls for organizations to, “Create joy in work by cultivating and mobilizing the pride and happiness of the health care workforce.” 5 The IHI now offers a variety of educational options for leaders to learn more about adopting Joy in Work strategies in their organization. In 2009, the IHI launched the “Joy in Work” initiative, 4 one of IHI’s 10 ways to radically transform health care. To accomplish the Triple Aim, the IHI recommends a change of process that includes identification of target populations, definition of system aims and measures, development of a portfolio of project work that is sufficiently strong to move system-level results, and rapid testing and scale-up that is adapted to local needs and conditions.
This is no small task it will require changing the overall clinical delivery model and the way physicians and other clinicians perform their duties (both individually and in teams), while supporting them with vastly improved informative data and resources (people and otherwise) to make the changes. Yet, to improve the health of our communities, the experience of patients and families, and slow the growth of health costs-and because it demands a systematic approach to improvement at all levels of the health care system-IHI contends that we need to address all three of the Triple Aim dimensions concurrently. Today, in most health care settings, no one is accountable for all three dimensions of the Triple Aim. It was also intended to help health care organizations focus on and redirect resources to activities that have the greatest impact on health. The premise behind the Triple Aim was that pursuing its three objectives at once allows health care organizations to identify and fix problems, such as poor coordination of care and overuse of medical services. 3 Our aging population and increased longevity, coupled with chronic health problems, have become a national challenge, putting new demands on medical and social services. The United States’ health care system is often referred to as the most costly in the world, with comparative analyses consistently suggesting that the United States underperforms on most dimensions of health care performance relative to other countries.

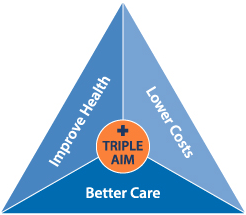
Since then, the Triple Aim has become an iconic moniker to represent the bar that health care strives to meet. As depicted in Figure 1, 1 the initiative was designed for health organizations to simultaneously pursue three dimensions 2: improving the health of populations improving the patient experience of care (including quality and satisfaction) and reducing the per capita cost of health care. In October 2007, the Institute for Healthcare Improvement (IHI) launched the Triple Aim Initiative.


 0 kommentar(er)
0 kommentar(er)
